Advanced imaging may be recommended during your appointment at Nashville Hip Institute at TOA (NHI at TOA). We carefully consider our patients’ specific needs and any previous imaging completed prior to recommending further diagnostic testing or imaging. We want our patients to understand why further imaging and/or diagnostic testing may be recommended.
The mission of NHI at TOA includes incorporating the latest in technology and imaging capabilities to accurately and efficiently diagnose and treat our patients. We want you to get back to your desired activities and lifestyle as swiftly as possible.
Please browse the links below to learn about some of these imaging techniques, and as always feel free to reach out directly to us with any questions.
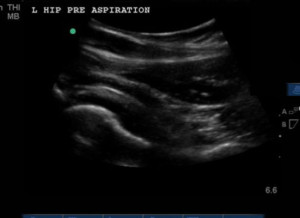
Ultrasonography
Over the recent years, ultrasound has really become an extremely useful device for diagnosing musculoskeletal injuries and damage as well as a convenient way for providers to guide needles into the joint and areas around the hip. The addition of ultrasound to our practice has really changed and advanced what we can do during your visit. NHI at TOA has been one of the leaders in developing ultrasound technology for the diagnosis and treatment of hip and pelvis disorders. A study performed here illustrated that these injections are significantly more convenient and less painful than fluoroscopic (x-ray) guided injections (Full Study Ultrasound-Guided Hip Injections: A Comparative Study With Fluoroscopy-Guided Injections).
During your ultrasound evaluation, a probe is placed on the skin along with some typically very cold gel. We promise we don’t put it in the refrigerator prior to your arrival. The probe uses sound waves to create pictures of the inside of your body, including the muscles, tendons, and joints in a safe, non-invasive manner. There is no radiation associated with the use of ultrasound. The real-time assessment we can perform during your visit gives your providers incredibly useful information to personalize an appropriate treatment plan.
Diagnosis
Ultrasound can be used to assess for many different hip related problems, encompassing both the joint and the surrounding soft tissues and bony structures. Having the capability to see where the exact area of damage is located allows: 1) the NHI at TOA physical therapists to more specifically outline rehabilitation recommendations, 2) the providers to know if you may have abnormal fluid collections indicating potential underlying problems, and 3) the surgeons to be aware of how much damage you may have prior to surgery. Below is a list of common hip and pelvic diagnoses we make with the assistance of an ultrasound exam.
- Muscle tears
- Tendinopathy
- Bursitis
- Snapping hip syndrome
- Joint effusion (excess fluid in the joint indicating irritation or infection)
- Ischiofemoral impingement
- Thickened joint capsule
- Scar tissue
- Muscle pain related to prominent surgical implants (such as a joint replacement)
Ultrasound Guided Procedures
During your visit at NHI at TOA, your provider may recommend an injection for diagnostic or therapeutic purposes. At times a diagnostic injection may be used to pin-point and isolate the source of your discomfort. Many times this will be completed after our physical therapist has completed an evaluation allowing us to know what causes discomfort, what is tolerated well, and strength deficits/dysfunction. Using ultrasound for needle guidance and/or identification of the area of damage, a numbing medicine is injected into your hip joint or the localized area of damage/pain. The medication should give close to immediate relief of any pain that is originating from the joint or tissue in question. The pain felt with activity and clinical examination prior to the injection should be evaluated following the injection. Knowing whether or not there is improvement while the area or joint is numb allows us to rule that area in or out as the primary contributor to pain and dysfunction.
Many times a second medication may be injected for therapeutic benefit. This can usually be injected at the same time as the numbing medication. A commonly injected therapeutic medication is a corticosteroid. In comparison to the anesthetic (numbing medicine), the steroid can take up to two weeks to work fully and the overall affects are highly variable. Some patients get a substantial amount of long term relief of pain (several months or more) while others may see no improvement. The benefit of using this type of medication is the ability to address soft tissue pain/restrictions, weakness and inhibition, and other non-hip related pain and dysfunction while the hip joint or soft tissues are not hurting or are less irritable. In addition to steroids, NHI at TOA also has the ability to inject platelet rich plasma (PRP), viscosupplements, amniotic allograft and stem cell products.
Some patients will do very well with conservative treatments (medication, therapy, etc.) and activity modifications while others may ultimately benefit from a surgical procedure. Either way, the injection allows for both diagnostic information to be collected as well as the opportunity to prepare an individual physically for the best possible rehab experience post op.
In addition to needle guidance for injections, ultrasound also gives us the ability to aspirate joints, morel lesions, bursal fluid, cystic lesions, and any other fluid collection around the hip area. The aspirated fluid can then be sent to the lab for assessment for underlying pathologic conditions.
Below are examples of ultrasound guided procedures commonly performed at NHI at TOA.
Ultrasound Hip Joint Injection
Iliopsoas Bursa Injection
Piriformis Injection
Ultrasound Guided Injection of Abductor Tear
Dynamic Assessment
While we have already discussed the use of ultrasound for getting real time images of the joint and surrounding structures, dynamic assessment can also be incredibly useful. What looks normal in a static state may not be normal in motion. Dynamic assessment can be utilized to look at your muscles and joints in motion. This allows us to see if muscles are moving normally, if bones or surrounding structures are “impinging” on each other, or if muscles/tendons are snapping.
Ischiofemoral Impingement
Snapping Iliopsoas
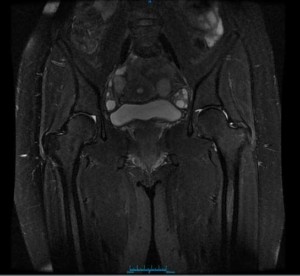
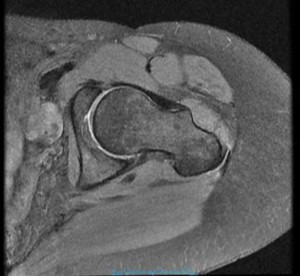
Magnetic Resonance Imaging (MRI)
MRI scans are frequently used to evaluate patients at NHI at TOA. MRI scanners use a powerful magnetic field and radio frequency to produce detailed images of your bones and soft tissues. It is very helpful in visualizing both damage and inflammation/fluid collections indicative of damage. Having an MRI does not expose the patient to radiation. This will require you to go to a facility close by but in many situation can still be completed the same day as your office visit. You may wonder why you need a scan when you have already had one somewhere else. The following are some key points and details we consider when deciding whether or not we need a new MRI.
- The MRI completed was performed produced low resolution images. We prefer MRIs complete on a 3T (Tesla) machine. This refers to the strength of the magnet used in the scanner. A standard MRI is completed on a 1.5T machine which, on average, produces lower quality images. If the images are low resolution we can have more difficulty assessing the amount of damage to smaller structures.
- The MRI completed was an arthrogram – meaning contrast was injected into the joint prior to the scan being completed. Contrasted MRIs can be useful for many reasons, but can also limit our ability to assess for certain types of problems around the hip. An irritable joint can sometimes create a buildup of fluid in the joint (an effusion). When contrast has been injected it is difficult to know how much joint fluid was present prior to the scan. Inflammation in bone and soft tissues can also be obscured by contrast in a scan. This type of inflammation can indicate numerous underlying problems including advancing arthritis and soft tissue injury that we would want to know about prior to recommending further treatment.
- The MRI was completed many months ago. Depending on what we are evaluating it can be crucial to have updated images. Some hip related problems can advance quickly and we want to make decisions based on recent information.
- The MRI completed did not have images of the specific hip in questions. Sometimes MRIs are completed of the whole pelvis instead of a specific joint. This provides a global view of the pelvis but doesn’t always allow us to see the joint in enough detail to make the necessary decisions.
When it comes to ordering diagnostic imaging, the providers at NHI at TOA will always try to limit the recommendations to what they feel is necessary and most beneficial to the patient. If you have further questions about the imaging ordered always feel free to ask the NHI at TOA team.
Computed Tomography Scan (CAT/CT scan)
The providers at NHI at TOA may suggest that you have a CT scan. This is basically a three dimensional x-ray of the bony structure. These are commonly ordered to evaluate possible fractures, look for bony deformities, and for surgical planning purposes. Like x-ray, CT scans do involve some radiation, but low dose protocols have been developed minimizing the amount necessary.
Location
2004 Hayes Street
Suite 700
Nashville, TN 37203
Office Hours
Monday-Friday:
8:00 am – 5:00 pm